What is Musculoskeletal Pain?
Musculoskeletal pain refers to discomfort or pain that affects the muscles, bones, tendons, ligaments, and nerves in the body. It can result from various causes, including injuries, overuse, or conditions like arthritis. Common symptoms include aching, stiffness, and tenderness in specific areas. This type of pain can be acute, coming on suddenly, or chronic, lasting for a long time. Effective treatment often includes rest, physical therapy, and medications to relieve pain and improve mobility.
Causes of Musculoskeletal Pain?
Musculoskeletal pain is one of the most common symptoms with which patients present in clinic. It can be due to variety of causes some of which are:
- Post traumatic
- Degenerative disorder
- Rheumatological disorder
- Osteoporosis
- Vitamin deficiency
- Infections
- Tumours
Post Traumatic musculoskeletal pain

Post traumatic musculoskeletal pain is easy to diagnose. Patient will present with history of injury and pain in the involved region. The origin of pain may be from bone, joints, ligaments, or muscles. There may be associated redness, rise of temperature and the involved part may be tender on touch. Immediately after injury patient should rest the injured part, do ice fomentation, compression bandage of swollen part to immobilise and decrease swelling and elevate the injured part/extremity (hence the acronym -RICE). Patient should immediately rush to an orthopaedic surgeon. Depending on the severity of injury and diagnosis, doctor may prescribe some tests. Bones and joint injuries will usually have a x ray whereas ligaments/ muscles will have MRI if required. If the injury is not severe, some anti-inflammatory drugs may be prescribed to alleviate pain and swelling. If there is a fracture/ joint dislocation/ torn ligament or muscle further intervention may be required.
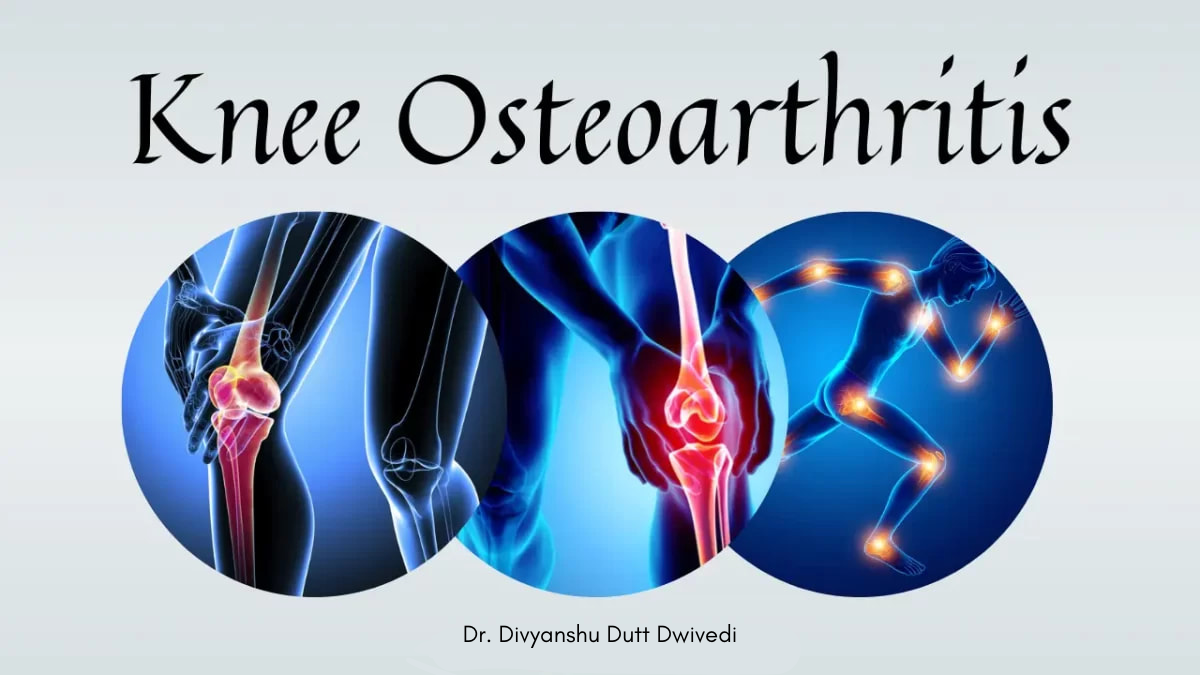
Degenerative disorder
It is also a common cause of musculoskeletal pain. Osteoarthritis of knee/ hip/ wrist/ hand, Cervical spondylosis, Lumbar spondylosis are amongst the most common degenerative disorders leading to pain. These disorders are mainly due to prolonged non physiological postures or inactivity. In the earlier cases brief period of medications, life style changes and exercising help in remission of pain. Advanced cases may require surgery of one kind or other.
Rheumatological disorder

The musculoskeletal pain may be due to rheumatological disease. These involve joints and other multiple organs in body due to uninhibited inflammation. Rheumatoid arthritis (RA), Ankylosing spondylitis (AS), Systemic lupus erythematosus (SLE), Psoriatic arthropathy, Gout etc. Rheumatoid arthritis and SLE are more commonly found in females whereas, AS is more in males. The Psoriatic arthropathy is associated with skin manifestations. All the above disorders usually have multiple joint involvement and have typical history of early morning stiffness which eases after a while. Rheumatoid arthritis involves more of hand joints/ knees. Ankylosing spondylitis involves more of back and hip. These disorders require prolonged medications to control inflammation (and thus other organ involvement) and advanced stages may require joint replacement.
Osteoporosis

With advancing average life span of humans, osteoporosis is already amongst the most common causes of musculoskeletal pain. Osteoporosis leads to loss of bone quality and quantity of bone tissue. Symptoms range from generalised bone pain to severe fracture related pain. Its is especially common in post-menopausal females. Osteoporotic fractures are commonly found in wrist, hip and back. Prompt diagnosis is paramount. A simple x ray like investigation called DEXA scan can easily diagnose osteoporosis. Healthy lifestyle, physical activity, good vitamin D intake in early stage is beneficial. Advanced stages will mostly need drugs to improve bone health. This therapy may be prolonged and should be supplemented with good diet and exercises.
Vitamin D deficiency

Vitamin deficiency, mainly vitamin D, can lead to bone pain especially in children. They are also associated thickening of the ankles, wrists and knees, bowed legs, soft skull bones and, rarely, bending of the spine in children. Chronic vitamin D deficiency can lead to early osteoporosis. The deficiency can have long lasting defects in skeleton and deformities may even require surgery. Simple weekly tablets/ sachets can treat this deficiency. The body naturally produces vitamin D when exposed to sunlight. Vitamin D rich diet such as oily fish, including salmon, mackerel, and sardines. Other sources are egg yolks, red meat, and liver.
Infections

Infections of bone and joint can lead to sever debilitating pain. They are associated with fever, immobilisation of involved body part, loss of appetite. These infections are usually emergency and should be seen by an orthopaedic surgeon as soon as possible. Severe infections may need surgical intervention to prevent long term sequalae/ deformities.
Tumours

They can also be uncommon cause of bone pain. The pain associated with tumours are usually severe at night. They may present with pain or may be preceded by swelling. Radiological diagnosis may be made by x ray/ CT or MRI. The biopsy may be taken to know the kind of tumour before proceeding to surgery in symptomatic cases.
Frequently Asked Questions
1. How to treat musculoskeletal pain at home?
Apply ice or a cold pack to the sore joint for 10 to 20 minutes at a time. Aim to do this every 1 to 2 hours while you’re awake for the next 3 days. Always place a thin cloth between the ice and your skin. After 2 or 3 days, you can switch to applying heat to the painful area.